Discovery of Specific Biomarkers Distinguishes Peri-Implantitis from Periodontitis
Researchers in oral health and implant dentistry are reporting promising advances in the molecular diagnosis of implant-related diseases. A growing body of evidence shows that specific biomarkers—measurable molecules in peri-implant crevicular fluid (PICF) or saliva—can help distinguish Peri‑implantitis (disease around dental implants) from Periodontitis (disease around natural teeth), offering a pathway toward earlier, more precise diagnosis and tailored treatment.
Key findings and context
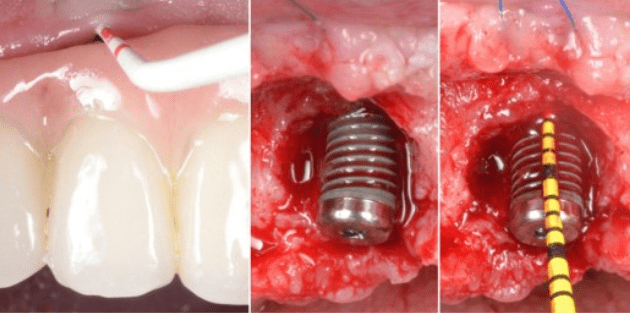
- Traditional diagnosis of peri-implant disease relies primarily on clinical indicators such as bleeding on probing, increased probing depth, and radiographic bone loss. However, these often reflect established damage rather than active disease states.
- A systematic review found that of 13 included studies comparing biomarkers in periodontitis vs peri-implantitis, nine reported significant differences in biomarker levels or biomarker ratios—most showing higher levels in peri-implantitis than in periodontitis.
- For example, levels of inflammatory cytokines (such as IL-1β, TNF-α) and enzymes involved in tissue breakdown (such as MMP-8) are consistently elevated in peri-implantitis compared with periodontitis.
- More recent work has focused on bone-remodelling markers: one study found that in PICF, the biomarker APRIL (a “A Proliferation-Inducing Ligand”) had a strong association with peri-implantitis—demonstrating good diagnostic performance when combined with clinical factors.
- Another recent review of oral-fluid biomarkers (saliva and peri-implant sulcular fluid) suggests that a subset of markers may reliably discriminate healthy implants from diseased implants—but the capability to distinguish implant disease from natural-tooth periodontitis is still under investigation.
Why this matters
- Implants are increasingly common and peri-implantitis can lead to implant failure or bone loss if diagnosis is delayed. Earlier detection via biomarkers could enable intervention before major damage occurs.
- Differentiating implant-site disease from tooth-site disease is clinically important because the tissues (structurally and biologically) around implants differ from those around natural teeth, and thus the disease mechanisms may differ. The elevated biomarkers in peri-implantitis suggest distinct pathobiology rather than simply “periodontitis at an implant”.
- Molecular diagnostics could enable a precision-dentistry approach: screening of implant patients, monitoring disease activity, risk-stratification, tailoring therapy intensity, and potentially improving outcomes by intervening earlier.
Limitations & next steps
- Many of the studies to date are cross-sectional (single time point) and relatively small; they cannot yet prove causality or temporal progression of disease.
- There is heterogeneity in definitions, sampling methods (PICF vs sulcular fluid vs saliva), biomarker panels, and cut-offs between studies. This makes standardisation challenging.
- Although differences in biomarker levels between peri-implantitis and periodontitis have been observed, there is not yet a clinically validated diagnostic panel or point-of-care test specifically designed to distinguish the two.
- Future research is needed: longitudinal studies tracking implant patients over time; larger cohorts; standardized sampling and biomarker assays; and integration of biomarkers with clinical and radiographic data to build predictive models.
Outlook
Experts believe that as the field of “molecular implantology” matures, implant-site fluid biomarkers will become part of routine monitoring for implant patients—much as salivary biomarkers are emerging in periodontology. One can envisage chair-side diagnostic kits that measure selected biomarker ratios, giving dentists an early warning of risk or active disease in implants, distinct from periodontal disease around natural teeth.
For now, the evidence strongly signals that peri-implantitis is not simply identical to periodontitis and that unique biomarker signatures exist. With further validation, these could transform how implant-related disease is diagnosed, monitored and treated.