Vaginal Fungal Infections: Causes, Symptoms, and Treatment
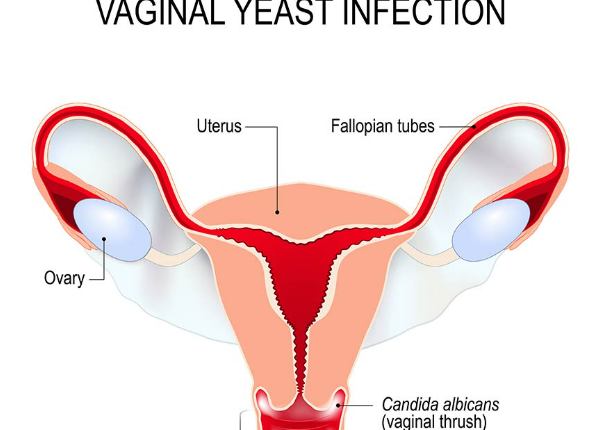
A vaginal fungal infection, commonly known as a yeast infection, is a common health condition experienced by many women. It occurs when the natural balance of bacteria and yeast (fungi) in the vagina is disrupted, leading to an overgrowth of yeast, most commonly Candida albicans. While not typically dangerous, vaginal yeast infections can be uncomfortable and recurrent if left untreated.
Causes of Vaginal Fungal Infections
- Imbalance in Vaginal Flora: The vagina naturally contains a mix of good bacteria (lactobacilli) and a small amount of yeast. When this balance is disrupted, yeast can multiply and cause infection. Factors that can disturb this balance include:
- Antibiotics: Antibiotics, while effective at treating bacterial infections, can also kill healthy bacteria in the vagina, allowing yeast to overgrow.
- Hormonal Changes: Pregnancy, menstruation, and hormone therapy can alter the balance of bacteria and yeast, increasing the risk of infection.
- Diabetes: Uncontrolled diabetes can lead to elevated blood sugar levels, which can encourage yeast growth.
- Weakened Immune System: Individuals with weakened immune systems, due to conditions like HIV or treatments like chemotherapy, are more prone to fungal infections.
- Tight or Non-Breathable Clothing: Wearing tight or non-breathable clothing, especially underwear made from synthetic materials, can trap moisture and heat, creating an environment where yeast thrives.
- Douching or Scented Products: Douching, as well as using scented soaps or feminine hygiene products, can disrupt the natural pH balance of the vagina, leading to an overgrowth of yeast.
Symptoms of Vaginal Fungal Infections
The symptoms of a vaginal yeast infection can range from mild to severe. Common signs include:
- Itching and Irritation: Intense itching and irritation in and around the vagina are hallmark symptoms.
- Burning Sensation: A burning feeling, especially during urination or intercourse, is common.
- Abnormal Discharge: Many women experience a thick, white, odorless discharge that resembles cottage cheese.
- Redness and Swelling: The vulva (the external part of the vagina) may appear red, swollen, and inflamed.
It’s important to note that symptoms of a yeast infection can sometimes be mistaken for other conditions, such as bacterial vaginosis or sexually transmitted infections (STIs). If you’re unsure, consult a healthcare provider for a proper diagnosis.
Treatment Options
- Over-the-Counter Antifungal Medications: Many mild yeast infections can be treated with over-the-counter antifungal creams, ointments, or suppositories. These medications, such as miconazole and clotrimazole, can usually clear up the infection within a few days.
- Prescription Antifungal Medications: In cases of severe or recurrent infections, your healthcare provider may prescribe stronger antifungal medications, such as fluconazole (a single-dose oral medication).
- Probiotics: Probiotics, particularly those containing lactobacillus, may help restore the balance of bacteria and yeast in the vagina. Some women find that taking probiotic supplements or consuming probiotic-rich foods like yogurt can prevent infections.
- Lifestyle and Prevention: Preventing yeast infections involves making certain lifestyle changes, such as:
- Wearing loose-fitting, breathable cotton underwear.
- Avoiding douching and scented feminine products.
- Maintaining good hygiene, especially during menstruation or after exercise.
- Managing blood sugar levels if you have diabetes.
- Limiting the use of antibiotics to when they are absolutely necessary.
When to See a Doctor
While yeast infections are generally not serious, you should consult a doctor if:
- This is your first yeast infection, as other conditions can mimic its symptoms.
- You experience frequent or recurring infections.
- Symptoms do not improve after treatment.
- You have unusual symptoms, such as a foul-smelling discharge, fever, or pelvic pain.
Conclusion
Vaginal fungal infections are common and treatable, but they can cause significant discomfort if left untreated. By understanding the causes, symptoms, and available treatments, women can manage and prevent these infections effectively. If you experience recurrent infections, it’s essential to seek medical advice to identify underlying causes and prevent further complications.