Understanding Psoriasis: Causes, Symptoms, and Management
Introduction
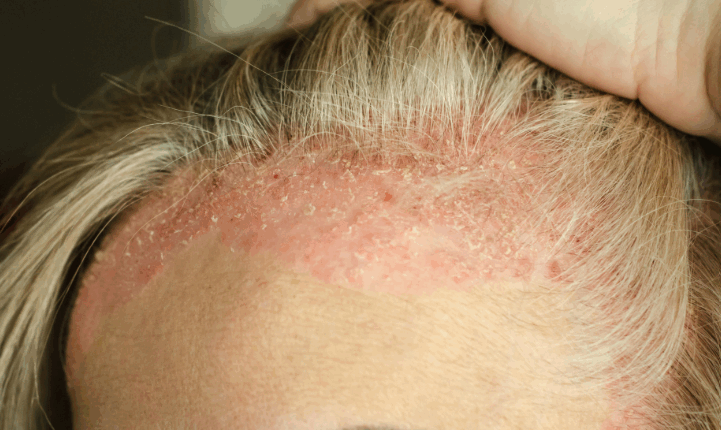
Psoriasis is a chronic autoimmune skin disease that affects millions of people worldwide. It is not contagious, but it can significantly impact a person’s physical and emotional well-being. Characterized by red, itchy, and scaly patches, psoriasis often appears on the scalp, elbows, knees, and lower back. Though it has no permanent cure, it can be effectively managed with the right treatment and lifestyle adjustments.
What Is Psoriasis?
Psoriasis occurs when the immune system causes skin cells to grow too quickly. Normally, skin cells take about a month to replace themselves. In people with psoriasis, this process happens in just a few days, resulting in a buildup of skin cells that form thick, scaly patches.
Types of Psoriasis:
There are several forms of psoriasis, including:
- Plaque Psoriasis (Psoriasis Vulgaris): The most common form, causing raised, inflamed red lesions covered by silvery-white scales.
- Guttate Psoriasis: Appears as small, dot-like lesions, often triggered by infections.
- Inverse Psoriasis: Occurs in skin folds like the armpits or groin, appearing as bright red, shiny lesions.
- Pustular Psoriasis: White pustules (blisters filled with non-infectious pus) surrounded by red skin.
- Erythrodermic Psoriasis: A severe, rare form causing widespread redness, itching, and pain across the body.
Causes and Triggers:
While the exact cause is unknown, several factors can contribute:
- Genetics: Family history increases the risk.
- Immune System: Autoimmune activity triggers inflammation and rapid skin cell turnover.
- Environmental Triggers: Such as stress, smoking, alcohol, certain medications, infections, and skin injuries.
- Weather Conditions: Cold and dry weather can worsen symptoms.
Common Symptoms:
- Red patches of skin covered with thick, silvery scales
- Dry, cracked skin that may bleed
- Itching, burning, or soreness
- Thickened or ridged nails
- Stiff and swollen joints (in psoriatic arthritis)
Diagnosis:
Psoriasis is typically diagnosed through physical examination and medical history. In some cases, a skin biopsy may be required to confirm the diagnosis and rule out other skin conditions.
Treatment Options:
- Topical Treatments
- Corticosteroids
- Vitamin D analogs
- Salicylic acid
- Coal tar
- Phototherapy
- UVB light therapy
- PUVA (psoralen + UVA light)
- Systemic Medications (for moderate to severe cases)
- Methotrexate
- Cyclosporine
- Biologics (e.g., adalimumab, etanercept, secukinumab)
- Lifestyle and Home Remedies
- Moisturizing regularly
- Managing stress
- Eating a healthy diet
- Avoiding triggers like alcohol and smoking
Living with Psoriasis:
While psoriasis can be a lifelong condition, many people manage it successfully. Support groups, therapy, and open conversations about the disease can help reduce the emotional toll and improve quality of life.
Conclusion:
Psoriasis is more than just a skin condition—it is a chronic, immune-related disorder that requires ongoing care and attention. With the right treatment strategy, medical guidance, and lifestyle choices, individuals with psoriasis can lead full, healthy lives. Raising awareness and educating the public about this often misunderstood disease is essential for early diagnosis, effective management, and better support for those affected.